With birth control coverage somewhat up in the air these days, an unlikely hero has emerged: the IUD.
The IUD, or intrauterine device, is a long-acting reversible contraceptive that has become more popular in recent years, particularly after the Affordable Care Act made it more accessible to women with insurance. They’re even the most popular birth control method among female family planning providers, according to a study in the journal Contraception.
IUDs received some free promotion after the presidential election, with people tweeting about getting the IUD to deal with their uncertainty about what health insurance and reproductive rights might look like over the next four years

After all, if you pop an IUD into your uterus now, you’ll be set for 3, 5, or even 10 years; the cost of staying baby-free won’t go up even if you lose your birth control coverage.
This idea seems to resonate with people. Recent data from WomanCare Global found that 21% of millennials in their survey considered getting an IUD in the past three months. Another survey from AthenaHealth and Vox found a 19% increase in doctor’s visits regarding IUDs after the presidential election.
So if you’re considering an IUD — whether you’re switching from another method or starting birth control for the first time — there are several important factors to consider.
BuzzFeed Health spoke with two board-certified gynecologists to get their advice: Dr. Mary Jane Minkin, clinical professor of obstetrics, gynecology, and reproductive science at Yale School of Medicine; and Dr. Candace Howe, of HM Medical in Newport Beach, California.
1. First things first, there are two types of IUDs: hormonal and non-hormonal.

The hormonal IUD is made of plastic and releases a small amount progestin (a synthetic hormone involved in menstruation and pregnancy) into the uterus. This helps prevent sperm from getting into the uterus and thickens cervical mucus to make it a hostile environment for sperm. It may also thin the lining of the uterus, making it harder for an egg to attach. There are a few brands of hormonal IUDs including:
* Mirena: the most popular one, which lasts up to five years.
* Skyla: a slightly smaller option with a little less progestin in it, which lasts up to three years.
* Liletta: a newer version that lasts up to three years.
* Kyleena: a newer version that lasts up to five years.
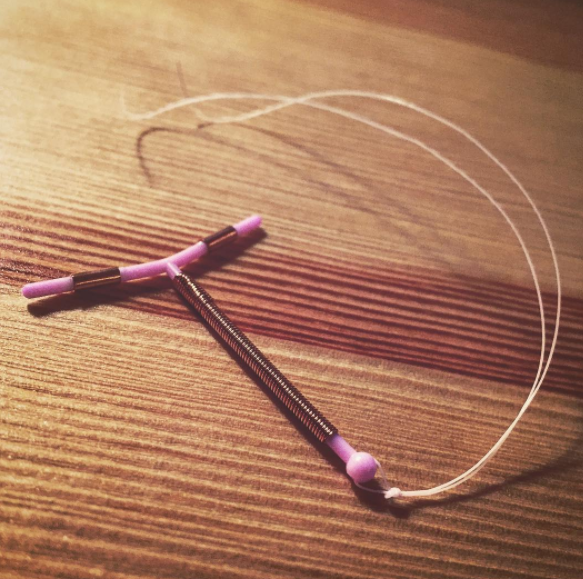
The copper (non-hormonal) IUD, called Paragard, is a plastic rod covered in a copper coil that releases copper into the uterus, producing an inflammatory reaction that makes it harder for sperm to move and survive in there. This method can last up to 10 years.
2. IUDs are so effective because they’re hard to mess up.
If you forget to take your pill every day or don’t always replace your birth control ring on time, an IUD is probably a good idea since it takes away the element of human error.
IUDs are over 99% effective, which basically mean you’re getting the effectiveness of female sterilization without the commitment, says Howe.
3. You can get an IUD whether you’ve given birth or not.
Even though the early IUD commercials called out mothers specifically, having a baby isn’t a prerequisite for this birth control.
This recommendation came from the fact that your uterus gets a little bigger after you’ve been pregnant, says Minkin, so it might be a little easier to insert an IUD in these people. But both experts agreed that all IUDs can fit in most uteruses — regardless of whether or not you’ve had a baby.
4. If you get really heavy periods, the hormonal IUD might be a good option.
If you run through a box of super tampons or heavy duty pads like it’s your job every month, the hormonal IUD can help with that. In fact, a lot of women stop getting their periods completely after a while, says Minkin.
That’s because the progestin being released from the IUD helps thin the lining of the uterus so there isn’t as much to shed each month, says Howe. However, both experts mentioned that the Skyla IUD might not lessen your periods as much as the others, since it contains less progestin.
5. The copper IUD, on the other hand, won’t do anything for a sucky period, so it’s a better option for someone who doesn’t really mind them.
Since the copper IUD is hormone-free, it won’t do anything to regulate your periods. In fact, some people report heavier, longer periods on Paragard, though that should let up after the first few months.
This is a major thing to keep in mind if, say, you started taking birth control pills as a teenager and now you’re considering an IUD, says Minkin. You might be able to think back to what your periods were like before you started birth control, but it’s also possible that your cycle changed over time. When you switch to a hormone-free method, you might be surprised by what your cycle is really like.
It could even reveal a hormonal imbalance (like hypothyroidism) or endocrine system disorder (like PCOS), says Howe, if your periods ran like clockwork while on hormonal birth control and are suddenly irregular after switching to a hormone-free method. If this happens, she suggests checking in with your doctor.
6. The IUD might be a better option for you than other birth control methods if you have certain health conditions or risk factors.

The copper IUD is obviously free of all hormones, so it’s a great option for someone who needs a long-lasting, non-hormonal birth control method; for instance, it’s recommended that people with a history of breast cancer avoid hormonal methods.
The hormonal IUD is also a good fit for certain people who can’t take combined birth control (ones that contain both estrogen and progestin), including people with a history of blood clots or stroke, high blood pressure (that isn’t well controlled), migraines with aura, and several other health conditions. It’s also recommended over birth control pills for anyone who is over 35 and also a smoker.
7. IUDs probably won’t help with acne and horrible PMS.
Fun fact: the hormonal IUD doesn’t actually stop you from ovulating. You’ll still experience the typical ups and downs of a regular menstrual cycle, but with a lighter (or nonexistent) period due to a much thinner lining of the uterus.
So if you suffer from bad PMS — cyclical mood changes or headaches, monthly breakouts, lots of bloating and discomfort — that will probably continue to happen with an IUD, whether you have the hormonal or copper one, says Minkin. This is also the case with premenstrual dysphoric disorder (PMDD) as well as mittelschmerz (pain during ovulation). That said, period cramps may be better with the hormonal IUD since your flow will be lighter, says Howe.
And while we know that combined birth control pills (with both estrogen and progestin) can help treat acne, that same effect hasn’t been shown for the hormonal IUD, which just contains progestin.
8. With the hormonal IUD, you’ll probably experience some spotting during the first three to six months.

So it might not be the best idea to get a hormonal IUD put in right before a big vacation, your wedding, or basically any time you’ll want to wear white. Be prepared to ruin a lot of underwear during this time, says Minkin.
This spotting between periods should lessen over time, but if you experience a lot of bleeding and it’s not letting up, be sure to check in with your doctor.
9. Your partner might feel the strings. It just happens.
Especially in the first few months, your partner may be able to feel the tips of the strings if they get near your cervix. Just give it some time, says Howe. Eventually, the strings will become a little softer and wrap up behind the cervix, so you won’t feel them unless you really go looking for them.
You could ask your doctor to trim them shorter, but that might make it a bit harder to remove the IUD when the time comes. Plus, shorter strings might end up poking your partner even more, says Howe, who recommends just leaving them be.
10. An IUD might be free under your insurance. But even if it’s not covered, it’s still a pretty cost effective option.
Under the Affordable Care Act, most insurance plans have to cover all FDA-approved methods of contraception at no cost (although they can choose to only cover the generic version). This applies to you whether you get your health insurance through your job or through the Marketplace, though there are some exceptions for grandfathered plans and religious employers.
Before you decide on an IUD, talk it over with your insurance company and your doctor to find out what’s covered. Without insurance, IUDs can be several hundred dollars. Still, $700 for a birth control method that lasts 60 months comes out to less than $12 a month.
11. Your doctor will typically want to schedule a consultation before they actually insert the IUD.

They’ll ask about your periods and medical history and discuss the different options you have available to you. “It’s not because I’m trying to discourage anybody, but it’s not an obvious choice,” says Minkin.
Once you’ve decided on a method, they’ll clear it with your insurance company and schedule a visit for the insertion. If possible, some doctors prefer to insert an IUD while you’re on your period, since your cervix opens up a little.
12. The insertion doesn’t take long, but it can range from mildly uncomfortable to very painful (depending on the person).

For the vast majority of people, the insertion will be a little crampy at times, and you’ll probably experience some cramping (like a bad period) for a few days afterwards, says Howe. Her biggest advice is to relax, take some ibuprofin before the appointment, and try not to tighten up.
Before you go, let your doctor know if routine pelvic exams are super painful for you; they may offer a numbing injection during your visit or have other suggestions, says Howe. And if you’re vasovagal (you tend to pass out when getting blood drawn, seeing blood, etc.), that could happen during insertion, says Minkin, so give your doctor a heads up and have someone drive you to and from your appointment.
Here’s a rundown of what happens during that IUD insertion visit:
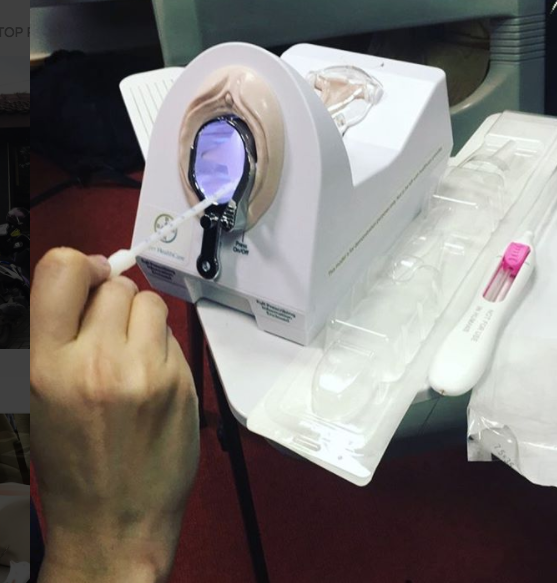
- First, you’ll typically get a pregnancy test and STI test (though you might not get a pregnancy test if you’re currently on your period).
- Then your doctor will do a pelvic exam to determine the shape and tilt of your uterus.
- They’ll insert a speculum (like they do during a Pap smear) and wash the cervix off with an antiseptic solution. Then they’ll grasp the cervix with little forceps to hold it in place during the procedure.
- Next, they have to measure the depth of the uterus by inserting a tiny metal rod called a sound. This tells them how deep they’re going to place the IUD.
- Finally, the IUD is inserted in a little tube with the arms tucked in, and they’ll use that tube to push the IUD into place in the uterine cavity, where the arms will extend.
- Once the IUD is in place, they’ll trim the strings to the right length, and you’re done!
Your doctor will also schedule a follow-up visit in four to six weeks to check in.
13. There are some risks associated with IUDs that, while rare, are important to talk to your doctor about.
During the insertion procedure, there’s a very small risk (1 in 1,000) of perforation, where the IUD penetrates the uterine wall or cervix, explains Howe. The risk of this is slightly higher in women who are lactating. If this happens (or if it migrates somewhere else), surgery may be necessary to remove it.
After the insertion, there’s about a 5% chance of partial or complete IUD expulsion, where the IUD is pushed out of place. Howe says the most common signs of this are bleeding and pain that isn’t getting better. This could decrease the effectiveness of the IUD, so it’s important to check in with your doctor if you’re experiencing any weird symptoms.
Finally, there is a very very tiny of risk of pregnancy with the IUD. But if you do get pregnant while you have an IUD, there’s a good chance it will be ectopic, meaning a fertilized egg implanted somewhere outside the uterus and cannot proceed. If the pregnancy is not ectopic, there is an increased risk of miscarriage unless you remove the IUD, says Minkin.
14. IUDs do not protect against STIs or HIV, so you’ll probably need to keep using condoms.
Unless you’re in a monogamous relationship and you’ve both been recently tested, the IUD is best used in conjunction with condoms.
It’s also super important to continue getting tested for any STIs you may be at risk for. That’s because untreated pelvic infections (like chlamydia and gonorrhea) can lead to pelvic inflammatory disease (PID), which can be particularly dangerous when you have an IUD in place, and it can lead to scarring and infertility if untreated. Symptoms of PID can include pelvic pain, bleeding, fever, and unusual discharge. See your doctor immediately if you experience any of these, says Howe.
15. Obviously IUDs aren’t for everyone.
As we’ve discussed, IUDs might not be the best choice for someone who gets really bad PMS, who also wants their birth control to fight acne, or who likes the reassurance that comes with a monthly period (hey, some people miss it when it’s not there!).
In addition to that, there are some cases where you should not get an IUD, for instance:
* If you’re pregnant.
* If you have uterine abnormalities that make it hard for the IUD to stay in place.
* If you have unexplained vaginal bleeding.
* If you have liver disease, a liver tumor, or cancer of the uterus or cervix
* If you have pelvic inflammatory disease (PID) or a history of PID, you might not be a good candidate for an IUD, but talk to your doctor about your history.
* If you have untreated pelvic infections (like chlamydia or gonorrhea) or are at a high risk of these infections, you might not be a good candidate for an IUD. Talk to your doctor about your risks.
* If you have breast cancer or a history of breast cancer, you cannot use the hormonalIUD.
* If you have Wilson’s disease (a rare disorder related to how the body handles copper), you cannot use the copper IUD.
16. IUDs can be taken out by your doctor at any time, and it’s possible to get pregnant as soon as they’re out.

You don’t need to wait 3, 5, or 10 years before taking your IUD out. If, for whatever reason, you’re done with it, just make an appointment with your gynecologist and they’ll remove it for you.
Minkin swears this part is easier and less painful than the insertion: they just grasp the strings with a little instrument and pull it out; the IUD arms fold upward to allow it to come down easily.
Keep in mind that you can get pregnant as soon as the IUD is removed, so if that’s not on the agenda for you, you’ll need to lock down another form of birth control.
The bottom line: The IUD might be a great choice for you…or it might not be. Birth control is not one-size-fits-all.
Before you decide on a method — even if it sounds like the best option ever — talk to your doctor about your health, your lifestyle, your insurance, and all your wants and needs from a birth control. They’ll help you decide which method is right for you.
And if you’re not sold on the IUD but you still want a long-acting method, don’t forget about the contraceptive implant, which is also over 99% effective at preventing pregnancy.
Via Buzzfeed

